Introduction to Rigid Bronchoscopy
What is a Rigid Bronchoscopy?
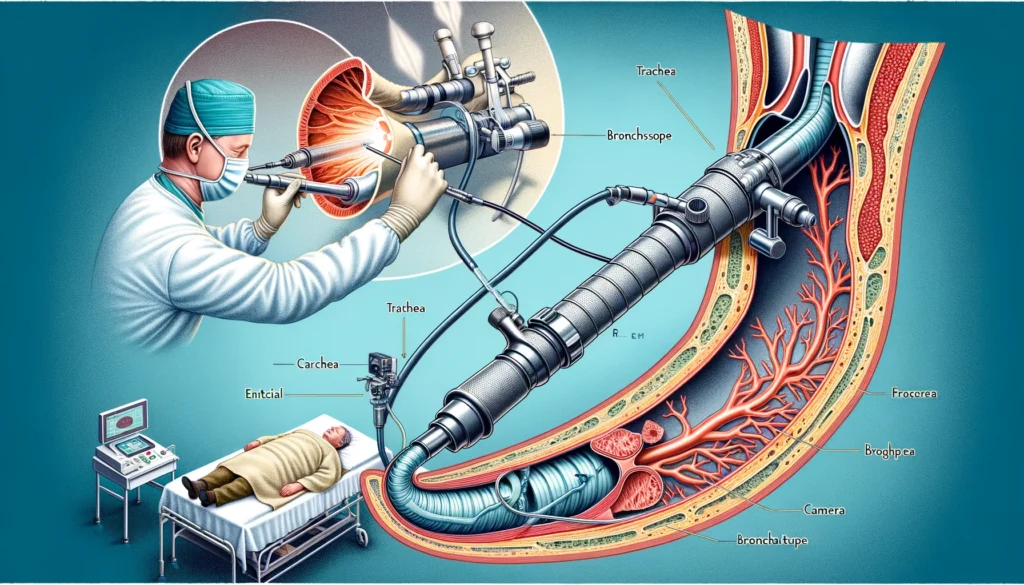
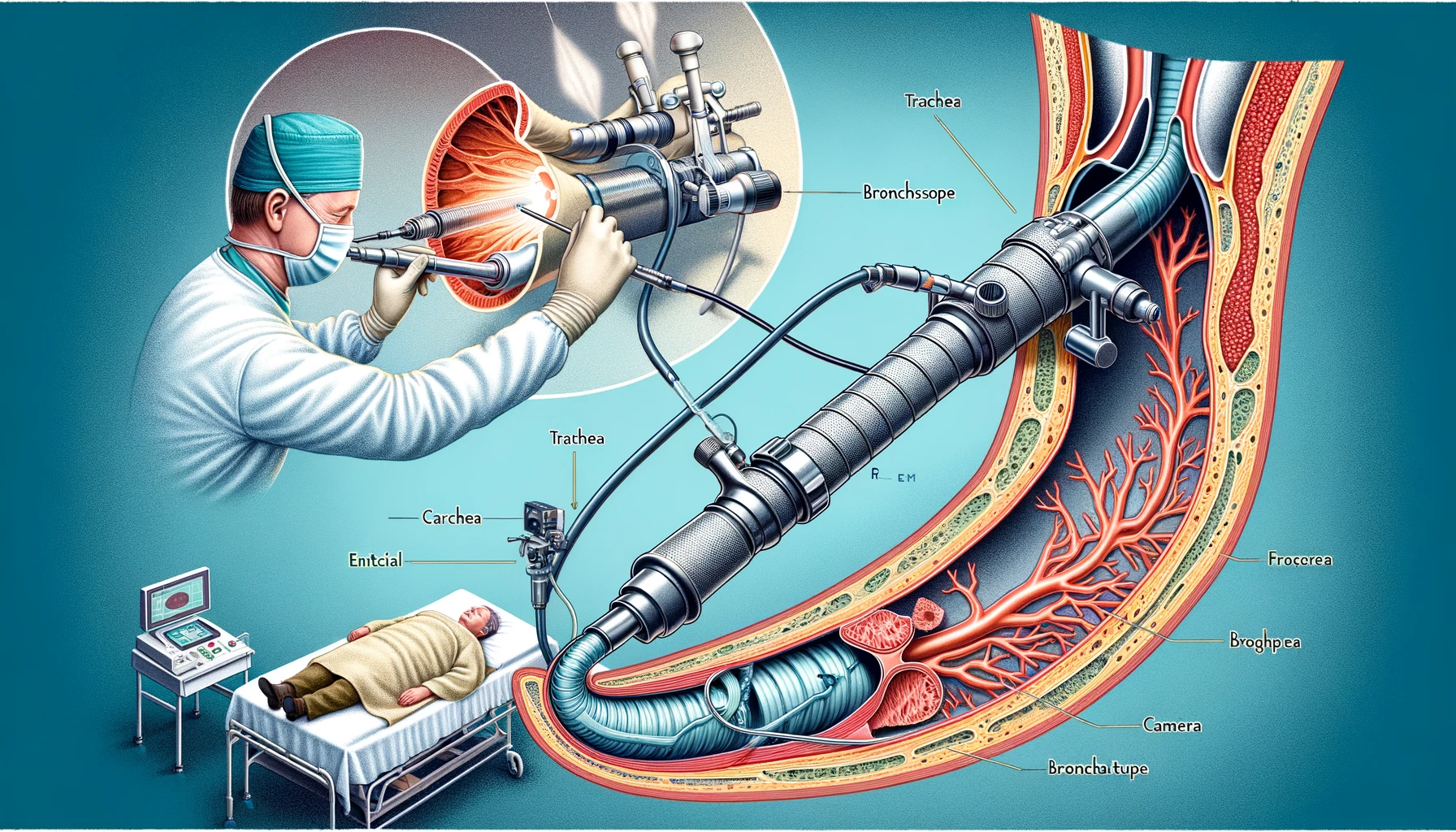
Rigid bronchoscopy is a specialized medical procedure that involves using a rigid bronchoscope to examine the lungs’ airways. This instrument is a straight, hollow tube equipped with a light and camera at its end, enabling doctors to visualize the trachea and bronchi directly. Unlike flexible bronchoscopy, which utilizes a more pliable scope, rigid bronchoscopy offers a more stable and larger working channel, making it particularly useful for certain diagnostic and therapeutic interventions. This procedure is essential for tasks requiring substantial airway control, such as removing foreign bodies, biopsy of suspicious lesions, stent placement, and managing central airway obstructions.
Historical Background
The roots of rigid bronchoscopy trace back to the late 19th century. In 1897, Dr. Gustav Killian performed the first bronchoscopy, marking a significant milestone in medical history. Over the decades, rigid bronchoscopy has evolved with advancements in technology and medical practices, enhancing its efficacy and safety. Initially, the procedure was primarily used for diagnostic purposes, such as inspecting the airways and identifying abnormalities. However, rigid bronchoscopy became a vital therapeutic tool as technology progressed. Its ability to provide a direct and unhindered view of the airways has made it indispensable in pulmonology and thoracic surgery.
Importance in Modern Medicine
In contemporary medical practice, rigid bronchoscopy is critical, especially in situations requiring immediate and precise intervention. Its significance is highlighted in emergency settings and critical care, where maintaining airway patency is crucial. Rigid bronchoscopy is often the preferred method for dealing with central airway obstructions, massive hemoptysis (bleeding), and complex therapeutic procedures requiring a stable and large working channel. The procedure’s ability to facilitate diagnostic and therapeutic interventions makes it a cornerstone in managing various respiratory conditions. As medical technology advances, rigid bronchoscopy remains a vital tool, contributing to improved patient outcomes and the advancement of respiratory care.
Indications for Rigid Bronchoscopy
Diagnostic Indications
Rigid bronchoscopy is frequently employed for diagnostic purposes in various clinical scenarios. It is particularly useful in obtaining tissue biopsies from the trachea and bronchi to diagnose lung cancers, infections, and other respiratory diseases. Additionally, it allows for direct visualization and assessment of airway abnormalities such as tumors, strictures, or congenital anomalies. In cases where imaging techniques such as CT scans or X-rays show ambiguous results, rigid bronchoscopy provides a more definitive evaluation, enabling clinicians to make accurate diagnoses and plan appropriate treatments.
Therapeutic Indications
Beyond its diagnostic utility, rigid bronchoscopy plays a crucial therapeutic role. It is the procedure of choice for removing foreign bodies lodged in the airways, a common occurrence in pediatric cases. The rigid scope’s large lumen and stable structure make it ideal for manipulating and extracting objects that flexible bronchoscopes cannot handle as effectively. Furthermore, rigid bronchoscopy manages airway obstructions caused by tumors, benign growths, or scar tissues. It facilitates the placement of stents to keep the airways open and allows for laser therapy or mechanical debulking of obstructive lesions, providing immediate relief to patients with compromised airways.
Contraindications
Despite its benefits, rigid bronchoscopy is not suitable for every patient. Contraindications include severe hypoxia, uncontrolled bleeding disorders, and unstable cardiovascular conditions, as these factors can increase the risks associated with the procedure. Patients with significant cervical spine instability or severe tracheal stenosis may also be poor candidates due to the potential for airway trauma. A thorough pre-procedural assessment is essential to identify these contraindications and mitigate the risk of complications. Additionally, careful consideration must be given to the patient’s overall health status and the potential benefits and risks of performing the procedure.
Procedure Overview
Pre-procedural Preparation
Proper preparation is critical to the success and safety of a rigid bronchoscopy. Pre-procedural steps include a detailed medical history and physical examination to identify potential contraindications. Blood tests, including coagulation profiles, are performed to ensure the patient’s readiness for the procedure. Patients are typically required to fast for several hours before the bronchoscopy to reduce the risk of aspiration during anesthesia. The procedure is usually performed under general anesthesia, so pre-anesthetic evaluation and planning are crucial. After discussing the risks, benefits, and available options with the patient, informed consent is acquired.
Step-by-Step Procedure
The rigid bronchoscopy procedure begins with the patient being positioned supine with the neck slightly extended to facilitate airway access. After the induction of general anesthesia, the rigid bronchoscope is carefully inserted through the mouth and advanced into the trachea. Continuous visualization is maintained using a camera attached to the scope. The bronchoscope allows for direct inspection of the tracheobronchial tree, and any abnormalities are noted. Depending on the indication, biopsies may be taken, foreign bodies removed, or therapeutic interventions such as stent placements or laser treatments performed. The procedure is meticulously monitored to ensure patient safety and effective airway management.
Post-procedural Care
Post-procedural care is vital to monitor and address any complications that may arise following a rigid bronchoscopy. Patients are observed in a recovery area until they regain full consciousness and their vital signs stabilize. Potential complications such as bleeding, infection, or respiratory distress are closely monitored. Pain management and supportive care, including oxygen therapy if needed, are provided based on the patient’s condition. Follow-up appointments are scheduled to assess the patient’s recovery and the success of the intervention. Patients are advised to report any persistent or worsening symptoms, such as difficulty breathing or chest pain, to their healthcare provider immediately.



2 thoughts on “Rigid Bronchoscopy: 5 Essential Benefits of Advanced Airway Management”